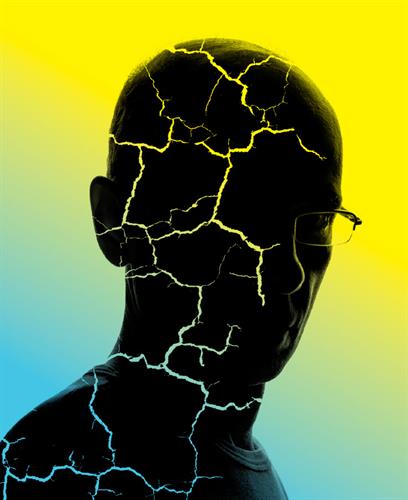
Cravings, Control and Consequences
Research on addiction is unearthing startling revelations.
By Maureen Salamon
 Addiction researchers have been eyeing the snowballing trend of declining American life expectancy—driven largely by drug overdoses and alcoholism—long enough to share terminology for the phenomenon.
Addiction researchers have been eyeing the snowballing trend of declining American life expectancy—driven largely by drug overdoses and alcoholism—long enough to share terminology for the phenomenon.
“We call it ‘deaths of despair,’ with the idea that it’s mostly due to underlying sociological factors related to the despair younger populations are feeling and coinciding with the availability of drugs to such an extent that they accidently or otherwise end up overdosing,” says Elyssa Margolis, PhD, who holds an endowed chair in genetics of addiction in neurology at University of California-San Francisco (UCSF) Weill Institute for Neurosciences.
The statistics are sobering. A November 2019 study in JAMA found the chances of dying of any cause before age 65 have climbed, with overall life expectancy dropping over the past three years after six decades of only gains. Leading contributors include a rise in deaths among working-age adults ages 25 to 64 due to overdoses and alcohol abuse, among other causes. Meanwhile, a January 2020 study in Alcoholism: Clinical & Experimental Research showed alcohol-related deaths in the U.S. are at an all-time high, doubling since 1999.
These alarming developments also underscore the vital need for physiology research into how and why the brain and body react as they do to addictive substances such as drugs, alcohol or even food. But the disconnect between lab science and actual individuals struggling with addiction can be “a tough nut to crack,” Margolis notes. “Some of those disconnects can’t be surmounted, but it’s important for us who are bench researchers to keep that human condition in mind.”
Derived from the Latin term for “bound to” or “enslaved by,” addiction wraps in three key components: compulsive cravings for a substance, loss of control over its use and continued use despite damaging consequences. The causes of addictive behavior first came to scientists’ attention in the 1930s, with researchers typically splitting that focus into a logical timeline of “before”—how cells respond to substances, influencing the development of addiction—and “after”—observing the physiological ramifications of substance abuse on human health. Ideally, experts say, both vantage points will point toward proactive or preventive measures that can help individuals and society avert worst-case scenarios akin to the latest U.S. longevity statistics.
“Both arms of the equation are very important,” says Patricia Molina, MD, PhD, FAPS, the Richard Ashman Professor and Chair of the Department of Physiology and director of the Alcohol and Drug Abuse Center of Excellence at Louisiana State University. “One is trying to understand what makes the brain addicted to a drug, and a slew of investigators are focused on that.
“My work focuses on, if someone is using a substance, how that substance interferes with the biological processes critical for health,” says Molina, past president of the American Physiological Society. “My focus is understanding what happens beyond the brain.”
Evolving Beliefs
Margolis, who studies neural circuits involved in drug reinforcement and seeking, falls squarely into the “before” camp, and her work has generated controversial results. For example, her September 2017 paper in the journal Neuropharmacology used a variety of techniques—including animal models, electrophysiology and single gene expression assays—to examine mu and delta opioid brain receptor response to two opiates that supposedly activate the same receptor.
What she found “verged on heretical for the field,” Margolis says. “There was no relationship between the neural responses to the two compounds, even though in theory the two compounds were working on the same receptor. If you’re doing exactly the same thing and using the same receptors, cells should respond the same way to both drugs.
“This matches up really nicely with behavioral results because this means patients won’t develop cross-tolerance,” Margolis explains. “I’ve gotten a lot of pushback in the field because it makes things a lot more complicated. … On the other hand, a lot of effort is now going into designing molecules or doing screens for molecules that have this other property people are referring to as functional selectivity.”
Howard Fields, MD, PhD, UCSF professor emeritus of neurology and physiology, also explores the “before” side of addiction research. His more recent research zeroed in on reward pathways in the brain and how the neurotransmitter dopamine—key to the reinforcement of rewarding behaviors—influences motivation and choice.
In a 2014 study in the Journal of Neuroscience, Fields, Margolis and colleagues upended the dogma surrounding how dopamine works in the ventral tegmental section of the brain. Much research had established this region as essential to the rewarding and motivational action of opioids.
“What was new about this study was, yes, opioids work on this part of the brain, but they don’t work by the disinhibition mechanism everyone believed was true, i.e., that the direct effect of opioids was to inhibit inhibitory neurons and indirectly excite dopamine neurons,” Fields says. “We demonstrated that opioids can activate dopamine neurons directly. A lot of people still don’t believe it because the dogma was that the mechanism was indirect.”
While the study may not have produced concrete steps individuals can take to protect themselves against addiction, Fields is taking a longer view. “Hopefully, the major impact of our work will be to develop a safer opioid people can use for pain management and figure out better treatments for those who are already addicted,” he says.
Real-life Relevance
For some scientists, the decision to devote their careers to addiction research is—at least partially—personal. For Fields, a U.S. Army stint during the Vietnam War exposed him to wounded soldiers with painful nerve injuries, whom he felt compelled to help. For Ole Petersen, CBE, FRS, a professor in the School of Biosciences at Cardiff University in Wales, a hard-drinking father colored his impressions of alcohol and its power.
“I decided early on I wasn’t going to drink because I didn’t want to be like that,” says Petersen, also founding editor-in-chief of APS’ new journal, Function, launching this year. His research concentrates on the function of the exocrine pancreas and pathophysiology of acute pancreatitis, a condition in many cases caused by excess alcohol. To that end, Petersen’s body of work veers toward the “after” of substance abuse, though he doesn’t strictly consider himself an addiction researcher. “My impression is that the effects of alcohol on the brain may be somewhat less understood than in a relatively simple organ like the pancreas, where we now have a very detailed molecular understanding of how alcohol, in combination with fatty acids, damage the cells,” he says.
Lab work may often seem like it takes place far away from those touched by substance abuse, but Petersen contends that understanding the mechanisms of the toxic actions of alcohol on various organs is crucial to both clinicians and the public.
“For physicians, our research helps them speak to patients with more authority, which increases enormously if it’s very clearly seen and felt that they understand what’s happening,” he says. “There are multiple levels of influence outside finding a cure or effective treatment in disease. It’s very important to always understand why something works.
“When for example, advising to cut alcohol consumption, it helps if one can explain exactly why it’s toxic,” Petersen adds. “With regard to acute pancreatitis—which, if recurrent, dramatically increases the risk for developing pancreatic cancer—evidence-based preventive measures for what is effectively a lifestyle disease will become increasingly important.”
Aiming at Alcohol Abuse
Molina’s body of research, which examines the interaction between alcohol and other drugs of abuse with chronic disease—particularly HIV infection—will ideally lead to understandings that can cut alcohol use in this “very fragile” group, she says. Those with HIV experience alcoholism rates double that of the general population.
Her July 2018 study in the American Journal of Physiology—Endocrinology and Metabolism also produced unexpected insights. Examining the differential contribution of chronic binge drinking and antiretroviral therapy to metabolic dysfunction in SIV-infected (a model for human HIV) macaque monkeys, Molina and colleagues observed “significant alterations in muscle and mitochondrial function—the most fundamental energy source for the body”—despite rigorous infection control.
“What was really surprising was the fact that even when you control viral load, drinking has a significant impact on physiology,” Molina says. “You would not think that. You would think if the infection were controlled, everything else is going to be OK.”
Similarly, she says, someone with a more typical chronic condition such as high blood pressure, diabetes or cardiovascular disease might consider that their alcohol consumption is completely unrelated to their ailment “when that’s clearly not the case.” Molina hopes future research might reveal the intimate connections between heavy drinking and a host of downstream health effects.
“Alcohol and many other drugs of abuse can impact so many systems that will affect not only the progression of chronic diseases but can also affect responsiveness to treatment or delay how fast you will recover,” she says. “Alcohol will impair the way your bone heals after a fracture. Alcohol will maybe aggravate or accelerate the development of diabetes if you have prediabetic syndrome. So I feel that understanding what might be an OK amount of drinking for a healthy individual may not necessarily be an OK amount for someone with a chronic disease.”
Petersen and Molina agree that society still largely considers heavy drinking acceptable—a notion they say needs to be stamped out as firmly as tobacco use. Here, too, physiology research might prove pivotal.
“In campaigning against excessive intake of dangerous substances, including alcohol, it may be helpful if you can explain why it’s dangerous,” Petersen says. “If you know there’s a mechanism and you can explain exactly why, I think it helps people understand it’s a real phenomenon.”
The Physiologist Magazine
Read the Latest Issue
Don’t miss out on the latest topics in science and research.
View the Issue Archive
Catch up on all the issues of The Physiologist Magazine.
Contact Us
For questions, comments or to share your story ideas, email us or call 301.634.7314.


