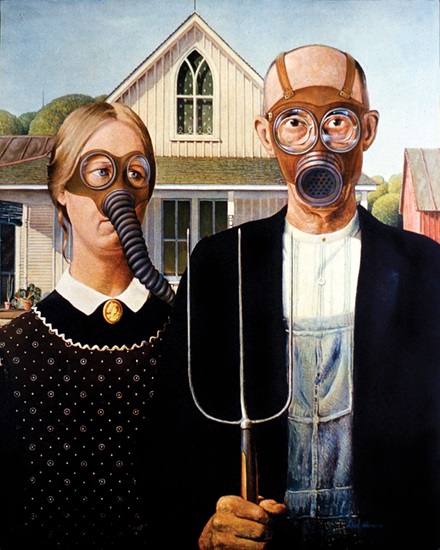
American Toxic
In the air and water, at work and at home, pollutants abound.
By Lauren Arcuri
From the air we breathe to the water we drink, from the food we eat to the places we work, humans and other animals are exposed to a wide variety of environmental pollutants that potentially endanger our health. While some toxic substances—such as arsenic—occur naturally, by and large, it’s human activity and technology that expose us to toxic pollutants.
Ambient air pollution is a major risk to human health. According to the World Health Organization, an estimated 6.2 million deaths occur each year worldwide due to air pollution, which we know causes cardiovascular disease and chronic respiratory illness. Air pollution is made up of a “heterogeneous mixture of different-sized particles in the air,” explains Loren Wold, PhD, FAPS, associate dean for research operations and compliance and professor of medicine and nursing at The Ohio State University.
There are thousands of different chemicals, gases and particulates that are considered “particulate matter.” They fall into three main categories by size: ultra-fine, fine and coarse. “Our interest is mainly in the fine particulates because they’re known to have the greatest effects on human health, and they’re the size predominantly produced by the combustion of fossil fuels,” Wold says. This category of particulate matter is 2.5 microns in diameter (PM2.5) and smaller.
Wold’s research began in the early 2000s, studying the effect of these small particles on the body in a mouse model. “We knew they affected the lungs, but our interest was: Is there potential for effects on other organ systems?” he says. “Initially, we started looking at the heart, and now we’ve branched into potential effects on brain health.”
Because elderly people are more likely to have heart disease, and make up the main population with Alzheimer’s disease, Wold’s lab wondered if there was a potential link between the two. Their hunch proved correct: “We’ve now shown that exposure to concentrated air particulates not only causes heart disease but can also potentiate early-onset neurodegenerative disease,” he says.
One of the prevailing theories of Alzheimer’s disease is that it is caused by changes in the brain’s vascular system. Research has shown that PM2.5 are small enough to pass through the endothelial lining in the lungs and into the bloodstream. Once in circulation, they can have direct effects on any organ system and can pass through the blood-brain barrier and impact the brain through the vascular network.
But Wold’s lab is interested in uncovering whether the particles could also be having a direct cardiac effect. “And then, is there a communication network between the heart and brain, what we call the heart-brain axis?” he says. “We don’t know what the communication network is yet, but we know there’s an inflammatory response with heart disease, and reactive oxygen species are produced. Both could potentially communicate to the brain.”
While the mechanisms of communication along the heart-brain axis are still under study, Wold’s lab has shown, in the mouse model, that exposure to these particulates leads to both heart disease and greater deposition of β-amyloid plaque in the brain. “What we think it is,” Wold says, “is a combination of both inflammation as well as the production of oxidative stress and the promotion of an oxidant environment that can lead to a whole host of diseases.”
Wold also studies the effects of burn pit exposure on veterans via a mouse model. The researchers have found effects not only on the exposed mice, but their offspring. “I think this is an area that is under-discussed,” he says. “There’s a lot of personal choice that we take when exposing ourselves to certain environments that could have dramatic effects on our future children.”
John Hollander, PhD, professor and assistant dean for professional programs in the School of Medicine at West Virginia University, also studies the effect of pollutants on offspring. Specifically, his research focuses on nanoparticulates, “anywhere from 1 to 100 nanometers in size,” he says. To study them, the lab aerosolizes the nanoparticles and administers them via the lungs.
While there are many nanoparticles out there, Hollander’s lab focuses on nanosized titanium dioxide, which has been recognized as a risk by the National Institute for Occupational Safety and Health. Nanosized titanium dioxide is found in many products, from white paint to processed foods such as salami to sunscreen and other cosmetics. “It’s virtually everywhere,” Hollander says. “Anything that has the ability to repel water, it can be used. And these materials are manufactured in a plant that deals with some kind of nanoparticulate.” So, not only are consumers affected, but workers may have particularly high exposure.
His lab found that these exposures affect cardiac function, which seems to be suppressed, affecting the ability of the heart to contract. To understand why the heart isn’t working optimally in the face of these exposures, Hollander’s team studies the function of the energy powerhouses of the cell, the mitochondria.
“We have found that when you acutely expose these animals, there is a pronounced decrease in mitochondrial function. Sometimes we see effects in certain subtypes of mitochondria; sometimes it affects multiple types and sometimes only one. But the effects are things such as a decrease in respiratory capacity within the mitochondria and enhanced permeability transition of the pore opening,” he says. “So, the mitochondria will go through an apoptotic program much more easily.” They’ve also seen changes in electron transport chain complex activity, suggesting that the mitochondrial dysfunction may be a result of that complex being impaired.
Hollander’s most recent work is focused on gestational exposure. In his model, the researchers are able to monitor the cardiac function of fetal pups in utero via echocardiography. In both mothers and pups, they see decreases in not only cardiac function, but mitochondrial function and bioenergetics.
“This has been really exciting for us,” Hollander says. “Our most recent work has been geared toward a phenomenon termed ‘mitochondrial programming.’ The hypothesis is that in utero, when the pregnant dam is exposed, it is impacting the mitochondria of the fetal pup such that they’re being reprogrammed.”
“I think it’s critical that as researchers we’re thinking about the whole person, the whole body, when we’re thinking about exposures.”
Tara Nordgren, PhD
While this can cause damage to the pup in utero, it might not always. Hollander and his colleagues hypothesized that even the healthy-appearing pups might have some undetected damage from their exposure. “When the mouse encounters a secondary insult later in life that challenges the bioenergetics of the heart, we wondered if the mouse might be worse off than a mouse without that fetal exposure,” he says.
“Our preliminary data suggest that this is the case. There are epigenetic changes that are occurring in utero. Those genes that are being epigenetically modified are changing such that down the road, the mitochondria have been reprogrammed to not be able to either tolerate or respond as appropriately to the secondary insults,” he says. Those secondary insults might be anything from an additional nanoparticle exposure to a known risk factor such as a high-fat diet.
Both Wold and Hollander’s research adds data to the hypothesis that pollutant exposure at the fine- and nano-level affects not only the animal directly exposed, but future generations.
POLLUTANTS IN THE WATER SUPPLY
Environmental pollutants are everywhere, including in our water supplies. And they’re not always put there by humans. Arsenic is a good example: While sometimes it’s in the soil from farming with pesticides and other human activity, it also simply occurs naturally in the earth’s crust, in higher proportion in some geographical areas than others.
If your water supply is municipal, your municipality likely tests for arsenic, making sure it’s at a safe level, generally under the Environmental Protection Agency standard of 10 parts per billion (ppb). “But if you look at many parts of the country and the world—people who are on well water in New England, many of the Plains states, and other countries in the world like Chile and Bangladesh—they tend to have levels that might exceed 500 or 1,000 ppb,” says Mark Kohr, PhD, associate professor of environmental health and engineering at Johns Hopkins Bloomberg School of Public Health in Maryland.
There is robust epidemiological evidence to suggest that both men and women suffer cardiovascular effects due to arsenic exposure. That said, “Arsenic doesn’t just affect the heart or cardiovascular system,” Kohr says. “It affects nearly every organ system in the body and has been labeled as a carcinogen.” Kohr’s lab looks at sex differences in cardiovascular disease, trying to understand the mechanisms that protect the female heart, at least until menopause. “So far,” he says, “we see strong sex-dependent effects with arsenic exposure. The adult male hearts are the most affected.” The female mice seem to be protected, at least during the short time frames Kohr has studied so far.
The arsenic-exposed male mice develop something called pathological hypertrophy: Their hearts get bigger and stronger, partly in response to an increase in blood pressure. “Although it’s initially a compensatory response and beneficial, eventually those mechanisms break down and it could culminate in heart failure.” While their studies haven’t yet shown heart failure due to their duration, Kohr says the development of this pathologic hypertrophy “is not a good sign for the males.”
Kohr’s lab is currently looking at gestational exposure to arsenic, trying to quantify its effects on cardiac development. “This project started because there’s a fair amount of literature that suggests that pregnant women exposed to arsenic might have a higher risk of having babies born with congenital heart defects,” he says.
Like Hollander, Kohr’s lab uses echocardiography to study the developing heart, and after the pups are born, they measure the heart’s function. So far, they do see some cardiac dimensional changes. There are impacts on the mother’s cardiovascular system as well, Kohr says. “There might be effects on maternal health here, too, which is a very understudied area. A lot of studies in both basic science and humans seem to focus on the health of the baby, but not the health of the mom.”
POLLUTANTS IN THE WORKPLACE
For many people, work is a place of potential pollutant exposure. More than 9 billion animals are raised for food each year in the U.S., the vast majority of them on concentrated animal feeding operations (CAFOs), according to the Natural Resources Defense Council. Epidemiological research over the past two decades establishes that CAFO workers, specifically hog farm workers, suffer health effects from dust in the air that contains endotoxins, fungi, microbes, ammonia, hydrogen sulfide and an array of other volatile organic compounds. Research has shown the dust also affects people who live near CAFOs.
While there is no shortage of epidemiological data showing that these environmental pollutants damage human health and cause various diseases, there’s a need for more basic research to help us understand more fully how this is happening.
An interdisciplinary team published a 2021 review in the American Journal of Physiology-Gastrointestinal and Liver Physiology that laid out the evidence for the mechanistic effects of environmental dust pollution on the human gut and how the gut and lungs are interconnected—how exposure via one body system, such as breathing in hog dust, might lead to effects on another system, such as gastrointestinal barrier function. That team is Tara Nordgren, PhD, assistant professor at Colorado State University in Colorado; Declan McCole, PhD, professor of biomedical sciences at the School of Medicine at the University of California, Riverside; and Meli’sa Crawford, PhD, a postdoc in McCole’s lab.
One route: When we breathe particles in, our lungs’ mucociliary escalator brushes them upward out of our airways and into our throats, then we swallow them into our stomachs and onward through the rest of our gastrointestinal system. But it’s possible that exposure to one system could cause effects in another body system in ways such as by promoting systemic inflammation and through other mechanisms yet to be discovered.
Research shows that CAFO farmers and farm workers experience chronic airway inflammation as well as gastrointestinal symptoms such as vomiting and diarrhea. “We wanted to know, how is that happening?” Crawford says. “Is it solely because of changes to the microbiome, or could it be something else?” A more permeable intestinal barrier sets the stage for inflammatory bowel disorders such as Crohn’s disease.
To better understand the mechanisms and physiology involved, the team used a prepared formula meant to mimic real-life exposure to the dust, called hog dust extract (HDE), in a mouse model. They exposed the mice intranasally to the HDE for a three-week period and found increases in intestinal barrier permeability and serum endotoxins, Crawford says. “This is indicative of systemic endotoxemia, so inflammation—and this is only after three weeks. So who knows what prolonged exposure could do.”
They also found some inflammatory markers upregulated in the intestine, including TNF-alpha, a cytokine that can signal the upregulation of other pro-inflammatory cytokines and cause leakiness of the gut barrier.
“So now, we’re looking at the gut microbiome, because if there’s an increase in serum endotoxins and intestinal permeability, that means the gut microbiome is also going to be affected by this,” Crawford says. They have already found a decrease in the abundance of one particular beneficial bacterium in the mouse gut microbiome. “Right now, we’re trying to figure out how the decreased abundance of this species contributes to the inflammatory effects we’re seeing after exposure,” Crawford says.
Nordgren’s focus is on how HDE affects the lungs. “We see quite dramatic lung inflammation with an acute exposure. And if we expose them over a period of 21 to 24 weeks, we see not only inflammation but fibrosis happening—really dramatic pathological consequences for these exposures in a long-term setting,” Nordgren says.
The collaboration between McCole and Crawford, who both work on the gut, and Nordgren, who studies the lungs, has been an especially fruitful one. It’s emphasized for them just how interconnected our body systems are, particularly when it comes to exposure to these tiny particles in our environment.
“I think it’s critical that as researchers we’re thinking about the whole person, the whole body, when we’re thinking about exposures,” Nordgren says.
As their research continues to unfold, they’re hoping to elucidate more connections along the gut-lung axis.
“This is a unique opportunity to really look at how these two organ systems are interacting to impact overall health,” Nordgren says.
POLLUTANTS THAT DON’T FADE AWAY
Persistent organic pollutants (POPs) are a varied family of environmental contaminants that are dispersed globally and known to stay in our bodies and the environment for a long time. They are found in our food, our air, and our household and commercial products. There are many POPs, but Jenny Bruin, PhD, associate professor of biology at Carleton University in Ontario, Canada, studies six major classes of them: dioxins, polychorinated biphenyls, organochlorine pesticides, organophosphate pesticides, flame retardants, and per- and polyfuoroalkyl substances.
Bruin studies how POPs affect β-cells, the pancreatic endocrine cells that regulate our glucose homeostasis. Her recently published review shows strong evidence that POPs contribute to β-cell dysfunction, impaired glucose homeostasis, and altered metabolic and oxidative stress pathways in islets. This supports epidemiological studies that establish that exposure to POPs increases diabetes risk. However, there are some significant gaps in the data that Bruin hopes her lab can begin to fill in.
“There’s evidence for all six classes that these pollutants have the potential to affect insulin secretion,” Bruin says. “We need more studies in different types of models, not just in immortalized β-cell lines, but the existing studies certainly are convincing that POPs have detrimental effects on β-cells.”
While the ways POPs affect the β-cell may differ, with some causing constant overstimulation and others impairing insulin release, the overarching theme is that there is consistent evidence that insulin secretion is disrupted.
Like other researchers who study environmental pollutants, Bruin’s lab is trying to determine the mechanism. How exactly are these pollutants exerting their effect on the β-cells? One of the pathways they’re investigating is the aryl hydrocarbon receptor (AhR) pathway, which is known to mediate most of the effects of the dioxin family of pollutants.
“We’ve demonstrated very clearly that the AhR pathway is activated in islets by exposure to pollutants,” Bruin says. “So we’re exploring the role of AhR in β-cells and how downstream molecules that are activated via AhR affect β-cell physiology. More specifically, we’re looking at some of the drug metabolism enzymes that are induced by that pathway. And what do those drug metabolism enzymes do in the islet? That’s something that hasn’t really been explored before.”
TIME FOR SOLUTIONS
Industrialization brought with it global environmental contamination. As humans have developed agricultural and manufacturing industries, we haven’t always understood what pollutants we were creating in the process, nor what effect they might have on us and the rest of the planet.
While there is no shortage of epidemiological data showing that these environmental pollutants damage human health and cause various diseases, there’s a need for more basic research to help us understand more fully how this is happening.
“I think if we can better understand the mechanisms, we will better know how to approach potential solutions to mitigating these effects,” Kohr says.
This article was originally published in the July 2022 issue of The Physiologist Magazine.
As humans have developed agricultural and manufacturing industries, we haven’t always understood what pollutants we were creating in the process, nor what effect they might have on us and the rest of the planet.
The Physiologist Magazine
Read the Latest Issue
Don’t miss out on the latest topics in science and research.
View the Issue Archive
Catch up on all the issues of The Physiologist Magazine.
Contact Us
For questions, comments or to share your story ideas, email us or call 301.634.7314.


