The Amazing Kidney
Physiologists are advancing what we know about the kidney and its functions.
By Dara Chadwick
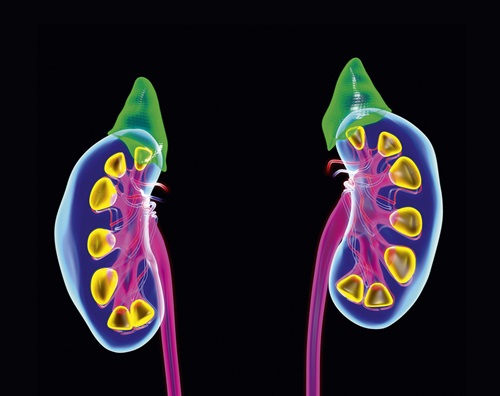
The kidney is one of the body’s most complex organs. Diverse cells within these fist-sized structures drive a mosaic of physiological processes. Our kidneys work constantly to filter blood, remove excess fluids and acids, and balance water, salt and minerals.
“It’s a fascinating organ,” says Heddwen L. Brooks, PhD, professor and chair of the Department of Physiology in the School of Medicine at Tulane University in New Orleans and editor-in-chief of American Journal of Physiology-Renal Physiology. “There are probably more than 100 cell types that make up your kidney.”
The kidneys—or more accurately, chronic kidney disease (CKD)—has a profound effect on the health and quality of life for many Americans. The Centers for Disease Control and Prevention (CDC) estimates that CKD affects about 37 million adults—more than 1 in 7—in the U.S. CKD is most prevalent in people over 65 (33.7%). The disease is also more prevalent in Black Americans (19.5%) than in non-Hispanic white Americans (11.7%).
Today, there is no cure for CKD. Controlling high blood pressure and diabetes can help stop the disease from progressing to end-stage renal disease. But many people who have CKD don’t experience symptoms until kidney damage is advanced. Lifestyle changes and current medications may not be enough to stop disease progression in some individuals.
Investigating the functions of kidney cells—with the goal of translating physiological research into clinical applications that could prevent or halt kidney disease—is happening in research labs across the globe. Here, we examine the latest research in renal physiology.
A Complex System
The kidneys control your blood pressure by sensing blood fluid content, excrete toxins and metabolize substances in a never-ending loop. It’s a delicate balance, according to Brooks.
Jennifer Pluznick, PhD, associate professor of physiology at the Johns Hopkins School of Medicine in Baltimore, studies olfactory receptors in the kidney. These G-protein-coupled receptors (GPCRs) help regulate sense of smell in your nose, but it turns out they’re also found in kidneys. “It sounds counterintuitive, but I encourage people to think of them as sensitive chemical sensors,” says Pluznick, an associate editor of AJP-Renal Physiology.
Pluznick began this research after a surprising finding while working with a kidney model. “I saw expression of olfactory receptors in a cell line where I didn’t expect to see them,” she says. “That was our first clue that olfactory receptors may be expressed in the kidney.”
Each GPCR seems to have a different role, Pluznick says. As an example, she cites olfactory receptors expressed in the renal tubule. “These receptors fine-tune renal transporters that play an important role in renal function.
Other GPCRs are expressed in the kidney’s vasculature, she says. “What’s interesting is all of them have a class of ligands in common,” she says. “These receptors and blood vessels are activated by a type of ligand produced by our gut bacteria. This has us thinking about how gut microbiota may affect kidney physiology and cardiovascular physiology.”
The kidneys also know what time it is and are regulated by circadian rhythms. Michelle Gumz, PhD, professor of physiology and aging at the University of Florida in Gainesville, was trying to identify early aldosterone target genes when she came across an interesting finding. A microarray of mouse kidney cells showed the most highly upregulated gene was a circadian rhythm gene called Period (PER) 1.
“We knew that kidney function had a circadian rhythm,” says Gumz, an associate editor of AJP-Renal Physiology. “But we didn’t know the mechanism of it. My hypothesis was that aldosterone induced the circadian PER1 protein that in turn regulated transport mechanisms in the kidney.”
Each cell type within the kidney has its own circadian clock, Gumz says. “We’re trying to figure out how these individual cellular clocks work together within the kidney—and how the clock in the kidney integrates with the clock in other tissues,” she says. “You want all the clocks throughout your body to be synchronized. But we don’t have a good handle on how these body clocks talk to each other.”
Generating knockout models is challenging because you can’t make a whole kidney where the clock gene is missing from every cell type. Gumz’s team creates transgenic models and challenges them in different ways, such as giving them a high-salt diet or eliminating dietary potassium. “What we find is there seems to be a connection between these clock proteins and salt sensitivity,” she says.
Gumz hopes her lab’s research may lead to clinical applications in personalized medicine. “Inherent circadian rhythm is different from person to person,” she says. “If we know more about the circadian clock and how it works in individual tissues and cell types, that could inform the use of circadian biology in treating patients, such as which drug to give and what time of day to give it.”
Unraveling the Kidney’s Mysteries
Jeff Sands, MD, FAPS, a nephrologist and emeritus professor at Emory University School of Medicine in Atlanta, studies urine concentration and dilution. His team is developing a novel therapy for a rare pediatric condition called congenital nephrogenic diabetes insipidus, or CNDI. Boys born with this X-linked disorder have a mutation in vasopressin receptor 2 (V2R) and produce up to 20 quarts of urine a day.
Sands and his team have explored ways to activate the protein and concentrate urine when the receptor is mutated. “We found a pathway we can target with novel therapeutics that may eventually lead to a therapy,” he says. “We’re in late preclinical development right now with the hope of getting to Phase I trials by the fall of 2024.”
In developing potential new therapies, the kidney’s complexity means off-target effects and unintended consequences can occur. Sometimes these effects are harmful, but sometimes they’re beneficial. Sands cites sodium-glucose cotransporter-2 (SGLT2) inhibitors as an example. “They were developed as a treatment for diabetes mellitus. But many of their beneficial effects are not what anyone thought they would be at the time the drugs were developed,” he says, noting their protective effects on the heart. “As a physiologist, you want to know why a drug that inhibits this transporter in the kidney leads to beneficial effects elsewhere.”
“Men and women can both develop kidney disease and hypertension, so understanding the role of sex as a biological variable is critical.”
Michelle Gumz, PhD
That complexity is part of what makes the kidney so fascinating to study, says Robert Fenton, PhD, professor in the Department of Biomedicine at Aarhus University in Denmark and APS Renal Section chair. “It’s difficult to understand one part of kidney function in isolation,” he says. “Whatever you change in one part of the kidney directly has an effect elsewhere in the kidney, which then maybe affects the vascular system, which then may feed back to the kidney.”
Fenton studies how the transport of ions and water affects kidney function. He and his team also examine the effects of kidney function on whole-body homeostasis, including the kidney’s role in maintaining blood pressure. High blood pressure and kidney disease can be complex, he notes.
“Over time, high blood pressure affects the blood vessels in the kidney,” he says. “They become damaged and narrow and don’t deliver oxygen and nutrients the kidney needs to function properly and repair. This limits their ability to compensate for damage from kidney disease, and the kidneys lose their ability to filter blood and regulate fluid and salts in the body. This drives blood pressure up, and then it’s a circular problem.”
Fenton’s lab explores how dietary interventions can help reduce blood pressure. “What we uncovered, alongside several other research groups, is that not only is blood pressure greatly influenced by sodium intake, but it is also influenced by dietary potassium intake,” he says. “There’s a negative correlation between dietary potassium intake and blood pressure. People that take in a potassium-deficient diet tend to have higher blood pressure and vice versa.”
Potassium can help the kidney switch from retaining sodium to excreting sodium, he says. “The overall consequence of this is a reduction in blood pressure,” he says.
Plenty to Discover
One area of potential advancement is diagnostics for kidney disease—particularly biomarkers. Today, Fenton says, biomarkers for kidney disease typically have predictive value only when disease is advanced, meaning about 50% of kidney function is already gone. “We’ve worked on trying to get a better diagnostic tool to study kidney disease,” he says. For example, a simple urine dipstick could alert users to see a doctor for further analysis.
Brooks also names biomarkers as a research area with potential for clinical application. “I think biomarkers are going to be important, but we also need to take sex into consideration when studying how the kidney works,” she says.
Brooks is focusing on how sex differences affect kidney cell function. Many kidney diseases are worse in men than in women, for example women are protected—compared to men—from conditions like acute kidney injury, chronic kidney disease and hypertension and resulting kidney damage.
Menopause shifts this protection, however. “In our studies, we’ve seen that in high blood pressure, males have more immune cells in their kidney than females, leading to higher inflammation, thus these cells seem to be contributing to the pathology,” Brooks says. Females are protected before menopause, with higher levels of anti-inflammatory immune cells, regulatory T-cells that may protect the kidney. “After menopause, when estrogen is no longer available, these specific cells are reduced, and this correlates with an increase in kidney damage and inflammation,” she says. “Our goal is to understand the physiology behind sex differences and a female’s resilience to kidney disease.”
Gumz says her team tries to conduct their experiments in groups of male animals and in groups of female animals. “What we’ve found is the responses to challenges and the effect of the knockout is different between the males and females,” she says. “Men and women can both develop kidney disease and hypertension, so understanding the role of sex as a biological variable is critical. We’re now working on looking at the mechanism of the clock in female kidneys in our mouse model to see what differences there are.”
Shuvo Roy, PhD, professor of bioengineering in the School of Pharmacy at the University of California in San Francisco, is developing an implantable bioartificial kidney that mimics the kidney’s natural physiology. “The vast majority of people with kidney failure rely on dialysis,” he says. “But there’s a physiological difference between dialysis function and our native kidney function.”
Filtration in the glomeruli is largely size based, Roy says. “Dialysis is fundamentally a diffusion-based process,” he says. “Its efficiency depends on the size of the molecule. Larger molecules move slowly, whereas in the convection or pressure-driven filtration of our kidneys, all molecules move faster and at the same speed. Dialysis has the complications it does because it doesn’t remove toxins as efficiently as our kidneys do.”
Roy’s device uses a biohybrid approach to mimic kidney physiology. Semiconductor silicon wafers create a mechanical hemofiltration unit, and engineered cadaver renal tubule cells create a bioreactor. The person’s blood pressure drives the filtration, so there’s no need for a battery or pump.
“Blood goes into the hemofilter and generates ultrafiltrate, just as the kidney does,” he says. “Ultrafiltrate then goes to a renal tubule-mimicking bioreactor, where engineered kidney cells process the ultrafiltrate, selectively transporting water and ions back into the bloodstream and producing urine. It’s not dialysis—it’s filtration followed by selective reabsorption.”
Roy sees potential for the device to get people to readily achieve 20% to 30% of kidney function, allowing them to avoid dialysis. He credits the pioneering work of physiologists in understanding kidney cell function as key to this effort.
“We have been inspired by physiologists and the fundamental kidney studies they’ve done,” Roy says.
This article was originally published in the March 2024 issue of The Physiologist Magazine. Copyright © 2024 by the American Physiological Society. Send questions or comments to tphysmag@physiology.org.
“It’s a fascinating organ. There are probably more than 100 cell types that make up your kidney.”
Heddwen L. Brooks, PhD
The Physiologist Magazine
Read the Latest Issue
Don’t miss out on the latest topics in science and research.
View the Issue Archive
Catch up on all the issues of The Physiologist Magazine.
Contact Us
For questions, comments or to share your story ideas, email us or call 301.634.7314.


