Diagnosing, Treating and Understanding Alzheimer’s Disease
There is hope on the horizon as research make great strides.
By Tyler Santora
Just five years ago, there was very little you could do if you were diagnosed with Alzheimer’s disease. You could try physical or cognitive therapy or a medication to manage symptoms. But you couldn’t stop the disease from progressing. Now, monoclonal antibody treatments offer the first hope at slowing the development of Alzheimer’s disease, a brain disorder in nearly 7 million Americans that causes memory loss and eventually the inability to carry out simple tasks.
“Patients can confidently feel that they’re doing something about a disease that previously all they could do was try to manage symptoms as best as possible,” says Gregory Jicha, MD, PhD, a professor of neurology at the University of Kentucky College of Medicine. “That’s a fundamental game-changer.”
Researchers have also made enormous progress in diagnosis. Before the early 2000s, Alzheimer’s disease could only be confirmed after death with autopsy. In the past couple of decades, however, scientists have developed ways to diagnose the disease by analyzing positron emission tomography (PET) scans and cerebrospinal fluid. But these tests are costly and resource-intensive—and most people would rather not have a spinal tap.
Simple blood tests for Alzheimer’s disease have revolutionized diagnosis since becoming clinically available in 2023. In addition to making it possible to screen large swaths of people, blood tests can also identify those with preclinical Alzheimer’s, meaning they’re in the very early, pre-symptomatic stages of the disease. Once these people are identified, clinicians can target them for lifestyle interventions. Clinical trials are even investigating whether the new monoclonal antibody treatments could delay or even prevent disease development in people with preclinical Alzheimer’s. And that’s just the beginning.
“I’m so excited about where we’re going to be 10 years from now,” Jicha says. “It’s going to be an incredibly different place, where Alzheimer’s remains a problem, but a chronic disease problem that is fully manageable with appropriate diagnosis and treatment.”
Blood Biomarkers
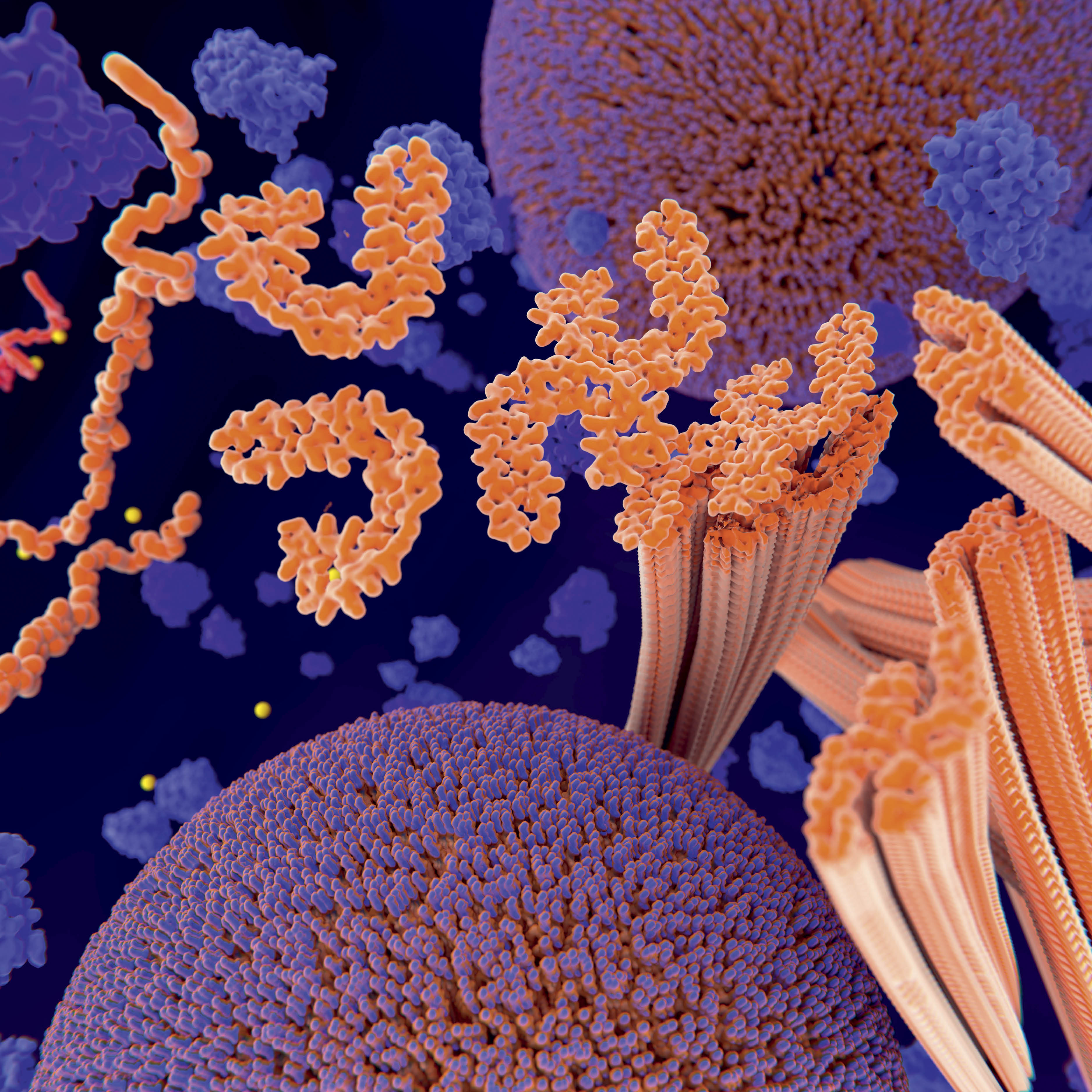
There are two major proteins that Alzheimer’s experts are concerned with: beta-amyloid and tau. In people with Alzheimer’s disease, beta-amyloid proteins clump together to form plaques that damage neurons and disrupt their communication. Levels of tau are often also increased in the Alzheimer’s brain, where they form tangles inside neurons and block communication.
New tests can accurately detect high levels of beta-amyloid and tau in the blood, years before a person develops Alzheimer’s symptoms. Because the tests are new, however, they may not be widely available, and not all insurance companies cover them. Experts expect that blood biomarker tests will become more accessible soon.
For now, positive blood test results require a cerebrospinal fluid test or PET scan to confirm diagnosis. More data over the near future will confirm the validity of the blood tests, determine which of the available tests is the most accurate, and assess how they’re being used clinically.
“In the next year or two, these will be much better understood,” Jicha says. “Our confidence in the ability to use them as less invasive and less costly biomarkers for the disease is going to become commonplace in medical practice.”
For now, clinicians are mostly using blood tests to determine whether an older person’s cognition issues are due to Alzheimer’s so that they can receive treatment. Soon, though, they could be used to detect people with preclinical Alzheimer’s so they can be offered preventive interventions.
“It’s a lot easier to preserve brain function than recover it after you’ve lost neurons, so that’s why people are really interested in using blood tests to look early,” says Jill Morris, PhD, an associate professor of neurology at the University of Kansas Medical Center and director of the University of Kansas Alzheimer’s Disease Research Center Developmental Projects Program.
Experts are also excited about the possibility of using blood tests to detect less infamous proteins that contribute to Alzheimer’s and related diseases. “There are so many other proteins circulating, and we’re getting more of a sense of what’s existing in the blood at certain times during disease processes,” says Rachel Buckley, PhD, an associate professor of neurology at Massachusetts General Hospital and Harvard Medical School.
Anti-Amyloid Treatments
Although experts don’t know what causes Alzheimer’s disease, there is a predominant theory: the amyloid hypothesis, which states that the disease is caused by accumulation of beta-amyloid in the brain. Because of this theory, researchers have been trying for the past 30 years to develop a therapy that targets beta-amyloid.
In 2021, they succeeded, with the first anti-amyloid therapy, aducanumab (Aduhelm), being introduced in the U.S. Although Aduhelm has since been discontinued by its manufacturer, two more anti-amyloid therapies have been added: donanemab (Kisunla) and lecanemab (Leqembi). These intravenous therapies work by removing beta-amyloid from the brain at different stages of plaque formation. They are monoclonal antibody therapies, or lab-made antibodies that bind to a specific disease-causing target, then recruit the immune system to destroy it.
These therapies aren’t perfect, however. For one, they only help people in the early stages of Alzheimer’s because they can’t reverse damage. Second, only a small percentage of people in the early stages are eligible for the treatments, largely due to chronic health conditions. Third, the treatments only slow progression by 30%.
“The next step will be, can we make them any better?” says Irina Skylar-Scott, MD, a clinical assistant professor of neurology and neurological sciences at Stanford University. One way to improve the treatments’ efficacy could be to give them to Alzheimer’s patients sooner, including in the preclinical stage—which has only become possible recently thanks to blood biomarker tests. Researchers are also investigating whether it could help to shuttle monoclonal antibodies past the blood-brain barrier directly into the brain itself.
Another important area of investigation is in decreasing the side effects of anti-amyloid treatments, namely amyloid-related imaging abnormalities, known as ARIA, which can cause brain bleeds and swelling. “Once we understand the basic physiology of the system, we can use adjuvant therapies that … reduce the incidence of this potentially lethal adverse effect,” Jicha says.
Experts like Jicha and Buckley are also excited about the possibility of combining anti-amyloid treatments with other therapies being developed and tested, including some promising anti-tau therapies.
Alternative treatments under development could help people who are ineligible for anti-amyloids. Jicha is looking forward to research on RNA silencers that could slow the production of beta-amyloid and tau to a level that the brain can naturally clear out on its own. This is currently being researched in people with Down syndrome who develop Alzheimer’s in midlife, but if successful it could be expanded to all people in the early stages of Alzheimer’s.
Researchers are also looking into whether anti-inflammatory therapies and GLP-1 drugs such as Ozempic could protect the brain against Alzheimer’s disease by altering the immune system and metabolism, respectively. However, there’s no real evidence in these areas yet, Buckley says.
Mind the Gender Gap
Nearly two out of three Americans with Alzheimer’s disease are women. Why is not entirely clear. One potential reason is that women live longer on average, so they have more time for Alzheimer’s to develop. Another is that women—and racial minorities, many of which have an increased Alzheimer’s risk—may be less likely to have modifiable risk factors such as high blood pressure addressed during midlife, Jicha explains.
The most important factors, however, are estrogen and menopause. Estrogen is a powerful sex hormone that protects the brain, so losing it through menopause is a shock to the system and puts women at risk. This is supported by the fact that women who start hormone therapy during perimenopause tend to decrease their risk of Alzheimer’s disease.
However, women who begin hormone therapy years after menopause increase their risk of Alzheimer’s, along with other diseases such as cancer, stroke and osteoporosis. This is particularly true in women who are already not at their healthiest. “Reintroducing a superpower like estrogen back into the body when it hasn’t had it for a while causes a whole bunch of things to go haywire,” Buckley explains. The body has already learned to compensate for the lack of estrogen, and adding it back could throw the body into chaos.
There are many other sex differences that affect Alzheimer’s disease: Women, even healthy women, have more tau than men. And women’s extra X chromosome may provide some risks and some protection against Alzheimer’s pathology. Also, APOE4, which is the strongest risk factor gene for Alzheimer’s disease, puts women at higher risk than men who have the gene. In addition, anti-amyloid treatments may be less effective in women.
None of these phenomena are well-understood. “There is just not enough data out there,” Buckley says. Studies on how sex differences, menopause and reproductive health affect women’s Alzheimer’s risk are few in number and small in size. “We have a lot more work to do.”
Prevention and Progression
Classic Alzheimer’s prevention advice remains the best: Follow an all-around healthy lifestyle. Keep your brain engaged, get enough sleep, stay social, exercise and eat a healthy diet. Vaccines that target tau, beta-amyloid and inflammation to prevent Alzheimer’s are in development too. “There are some promising candidates out there,” Jicha says. “But, of course, large-scale studies will need to be done, and there are always issues with balancing safety and immune responses and efficacy.”
For people who have already developed Alzheimer’s, lifestyle changes could slow progression, but more research is needed. “Once the disease develops, you have a lot of changes in the body and changes in the ability to function that might further affect disease progression,” Morris explains. For example, people with Alzheimer’s may be less likely to exercise, but it’s possible that physical activity could slow progression.
Therapeutic interventions coming down the pipeline could also slow Alzheimer’s progression, including anti-amyloid and RNA silencing therapies.
Zooming Out of the Neuron
“The field is shifting focus from just studying what’s happening in the neurons and [is now] looking broader inside the brain at what is happening to other cell types that could be contributing to the onset and acceleration of Alzheimer’s disease,” says Paulo Pires, PhD, an assistant professor of physiology at the University of Arizona College of Medicine-Tucson.
Pires is interested in how three other aspects of brain physiology contribute to Alzheimer’s. The first two are microglia and astrocytes. These are immune cells in the brain that can cause damage via multiple pathways, including by increasing inflammation, which can kill neurons and play a key role in Alzheimer’s pathology.
The third is the brain’s vascular system. Research is revealing how impairments in neurovascular coupling—changes to the vasculature in response to brain activity—may impair the delivery of nutrients to the brain and removal of its waste. This opens up the opportunity for therapeutics, as improving waste clearance could slow Alzheimer’s progression, although this hasn’t yet been well-studied, Pires says.
Morris is zooming out even further to look at the entire metabolic system. “We’re starting to realize that there’s bioenergetic changes throughout the body, specifically in non-brain tissues like muscle and liver, that might be important in the context of Alzheimer’s disease,” she says.
For instance, highly metabolic areas of the brain are among the first to accumulate amyloids, which signals to Morris that metabolic dysfunction may contribute to Alzheimer’s neuropathology. And research has shown that people with Alzheimer’s disease have impaired function of the energy-producing organelle mitochondria, so it could be a therapeutic target.
Between these emerging areas of research and the recent developments in diagnostics and therapeutics, the landscape of Alzheimer’s disease is fundamentally changing, for the better. “We all hope that this is the beginning and not the end of a new era for Alzheimer’s disease,” Skylar-Scott says.
This article was originally published in the January 2025 issue of The Physiologist Magazine. Copyright © 2025 by the American Physiological Society. Send questions or comments to tphysmag@physiology.org.
The Physiologist Magazine
Read the Latest Issue
Don’t miss out on the latest topics in science and research.
Contact Us
For questions, comments or to share your story ideas, email us or call 301.634.7314.